Chronic microvascular ischemic disorder is a term often used in the context of brain imaging findings, particularly on magnetic resonance imaging (MRI), to describe changes in the small blood vessels of the brain. It is commonly associated with small vessel disease (SVD), which involves the damage to the small arteries, arterioles, capillaries, and venules in the brain. These changes can lead to inadequate blood flow to certain areas of the brain, resulting in various symptoms. It’s important to note that chronic microvascular ischemic disorder itself is not a specific disease but rather a descriptive term for a pattern of changes observed on imaging studies.
or
Chronic microvascular ischemic disorder refers to a condition characterized by chronic, long-term impairment of small blood vessels in the brain, leading to reduced blood flow to certain areas. This condition is often associated with aging and other risk factors that contribute to the development of small vessel disease.
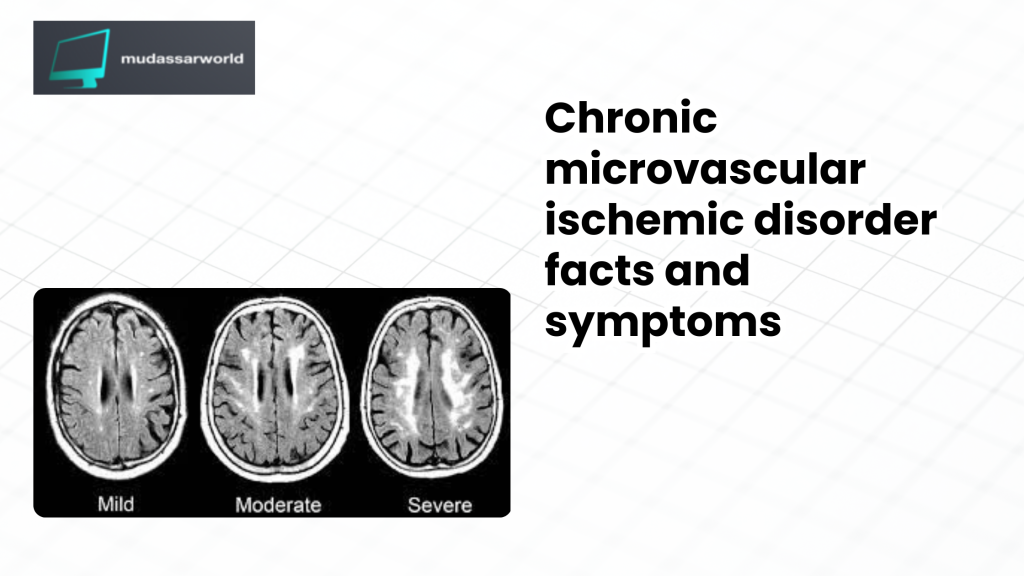
Table of Contents
Here are key points about chronic microvascular ischemic disorder:
- Small Vessel Disease (SVD): Chronic microvascular ischemic disorder is a type of small vessel disease that primarily affects the small arteries, arterioles, capillaries, and venules in the brain. These vessels play a crucial role in supplying oxygen and nutrients to different parts of the brain.
- Risk Factors:
- Age: The risk of microvascular ischemic disorder increases with age.
- Hypertension: High blood pressure is a significant risk factor.
- Diabetes: Individuals with diabetes are at an increased risk.
- Smoking: Tobacco use is associated with vascular damage.
- Hyperlipidemia: Elevated levels of cholesterol and triglycerides may contribute.
- Clinical Manifestations:
- Chronic microvascular ischemic disorder may be asymptomatic in its early stages.
- As the disease progresses, individuals may experience symptoms related to the affected brain regions, such as cognitive decline, memory problems, and issues with executive function.
- Radiological Findings:
- The condition is often identified through brain imaging studies, such as magnetic resonance imaging (MRI).
- Imaging may reveal white matter changes, small infarcts, or lacunar strokes, indicating compromised blood flow in the affected vessels.
- Management:
- Treatment focuses on managing underlying risk factors, such as controlling hypertension, managing diabetes, and promoting a healthy lifestyle.
- Medications, such as antiplatelet agents, may be prescribed to reduce the risk of blood clots.
- Prognosis:
- The prognosis can vary based on the severity of the condition and the extent of brain involvement.
- Lifestyle modifications and effective management of risk factors can slow the progression of the disease and improve outcomes.
It’s important for individuals with chronic microvascular ischemic disorder to work closely with healthcare professionals to manage their condition effectively. Regular monitoring, adherence to prescribed medications, and lifestyle modifications are crucial components of the overall management plan. If you or someone you know is experiencing symptoms suggestive of a neurological disorder, it’s essential to seek medical attention for a proper diagnosis and guidance on appropriate management.
Who does microvascular ischemic disease affect?
Microvascular ischemic disease, also known as small vessel disease (SVD), primarily affects the small blood vessels in the body, particularly those in the brain. While it can occur in various populations, it is more commonly associated with specific risk factors and demographic groups. Here are some factors that may increase the risk of microvascular ischemic disease:
- Age:
- Microvascular ischemic disease is more prevalent in older adults. As individuals age, the blood vessels can undergo changes, leading to reduced elasticity and increased susceptibility to damage.
- Hypertension (High Blood Pressure):
- Chronic high blood pressure is a significant risk factor for microvascular ischemic disease. Elevated blood pressure can damage the small blood vessels over time, leading to reduced blood flow.
- Diabetes:
- Individuals with diabetes are at an increased risk of developing microvascular complications, including damage to small blood vessels. Elevated blood sugar levels can contribute to vascular damage.
- Smoking:
- Tobacco smoke contains harmful substances that can damage blood vessels, contributing to the development of small vessel disease.
- Hyperlipidemia (High Cholesterol):
- Elevated levels of cholesterol and triglycerides in the blood can contribute to the formation of atherosclerosis (hardening and narrowing of the arteries), affecting both larger and smaller blood vessels.
- Cardiovascular Disease:
- Individuals with a history of cardiovascular diseases, such as coronary artery disease, may be at an increased risk of microvascular ischemic disease.
- Genetic Factors:
- There may be a genetic predisposition to small vessel disease. If individuals have a family history of vascular disorders, they may be at a higher risk.
- Ethnicity:
- Some studies suggest that certain ethnic groups may have a higher prevalence of microvascular ischemic disease. However, individual risk varies, and the impact of ethnicity is complex.
It’s important to note that while these factors are associated with an increased risk, microvascular ischemic disease can affect individuals who may not have these risk factors. Additionally, lifestyle factors such as diet, physical activity, and overall cardiovascular health play a role in the development and progression of small vessel disease.
Preventive measures, such as managing blood pressure, controlling diabetes, adopting a healthy lifestyle, and avoiding smoking, can contribute to reducing the risk of microvascular ischemic disease. Regular medical check-ups and early intervention for risk factors are essential components of maintaining vascular health. If you have concerns about your risk for microvascular ischemic disease, it’s advisable to consult with a healthcare professional for personalized guidance and preventive strategies.
How common is microvascular ischemic disease?
Microvascular ischemic disease, also known as small vessel disease (SVD), is a relatively common condition, especially in older populations. The prevalence of microvascular ischemic disease tends to increase with age, and it is often associated with other cardiovascular risk factors. The exact prevalence can vary based on the population studied, diagnostic criteria, and geographical location. Here are some key points regarding the prevalence of microvascular ischemic disease:
- Age-Related Prevalence:
- Microvascular ischemic disease is more commonly observed in older adults. As individuals age, the risk of vascular changes and small vessel disease increases.
- Common in Elderly Populations:
- Studies have shown that a significant proportion of elderly individuals may exhibit signs of microvascular ischemic disease on brain imaging, particularly on magnetic resonance imaging (MRI).
- Association with Other Risk Factors:
- Microvascular ischemic disease is often associated with cardiovascular risk factors such as hypertension, diabetes, smoking, and hyperlipidemia. Presence of these risk factors increases the likelihood of developing small vessel disease.
- Diagnostic Challenges:
- The diagnosis of microvascular ischemic disease is primarily based on imaging findings, and not all individuals with such changes on imaging may experience noticeable symptoms. As a result, the true prevalence may be underestimated.
- Geographical and Population Variations:
- The prevalence of microvascular ischemic disease can vary among different populations and regions. Genetic and environmental factors, as well as lifestyle choices, contribute to these variations.
- Underlying Health Conditions:
- Individuals with underlying health conditions, such as cardiovascular diseases or a history of strokes, may have an increased likelihood of microvascular ischemic disease.
It’s important to highlight that microvascular ischemic disease is often a part of the broader spectrum of cerebrovascular diseases. It may manifest as white matter changes on brain imaging, small infarcts, or lacunar strokes. The clinical significance of these findings can vary, and not everyone with imaging evidence of small vessel disease may experience noticeable symptoms.
As with any medical condition, early detection, management of risk factors, and appropriate medical care play crucial roles in minimizing the impact of microvascular ischemic disease. Regular health check-ups, especially for individuals at higher risk, can aid in the prevention and timely management of vascular issues. If you have concerns about your risk for microvascular ischemic disease, it’s recommended to consult with a healthcare professional for personalized assessment and guidance.
Symptoms and Causes
What causes microvascular ischemic disease?
Microvascular ischemic disease, also known as small vessel disease (SVD), involves damage to the small blood vessels in the body, particularly those in the brain. This condition can lead to reduced blood flow to various organs and tissues, with the brain being a common target. The exact cause of microvascular ischemic disease is multifactorial, and several factors may contribute to its development. Additionally, the symptoms associated with microvascular ischemic disease can vary depending on the affected organs.
Causes of Microvascular Ischemic Disease:
- Hypertension (High Blood Pressure):
- Chronic high blood pressure is a major risk factor for microvascular ischemic disease. Elevated blood pressure can lead to structural changes in the small blood vessels, making them more susceptible to damage.
- Atherosclerosis:
- Atherosclerosis involves the accumulation of plaque (fats, cholesterol, and other substances) in the arteries, leading to the narrowing and hardening of blood vessels. Small arteries and arterioles may be affected, contributing to microvascular ischemic disease.
- Diabetes:
- Diabetes is associated with damage to blood vessels throughout the body. Elevated blood sugar levels can lead to endothelial dysfunction and structural changes in small vessels, contributing to microvascular complications.
- Smoking:
- Tobacco smoke contains harmful substances that can damage blood vessels. Smoking is a significant risk factor for small vessel disease and can contribute to the development of microvascular ischemic disease.
- Hyperlipidemia (High Cholesterol):
- Elevated levels of cholesterol and triglycerides in the blood can contribute to atherosclerosis and the development of microvascular complications.
- Aging:
- The risk of microvascular ischemic disease increases with age. Aging is associated with changes in blood vessels, including reduced elasticity and increased vulnerability to damage.
- Genetic Factors:
- There may be a genetic predisposition to small vessel disease. Individuals with a family history of vascular disorders may have an increased risk.
Symptoms of Microvascular Ischemic Disease:
The symptoms of microvascular ischemic disease can vary based on the organs affected. In the context of the brain, common symptoms include:
- Cognitive Impairment:
- Memory loss
- Difficulty concentrating
- Slowed thinking
- Mood and Emotional Changes:
- Mood swings
- Depression
- Irritability
- Motor Function Issues:
- Problems with coordination and balance
- Gait disturbances
- Headaches:
- Chronic headaches, sometimes described as tension-type headaches
- Urinary Symptoms:
- Incontinence or urgency
It’s important to note that these symptoms can be nonspecific, and the severity may vary among individuals. A definitive diagnosis often requires clinical evaluation, imaging studies (such as MRI), and consideration of risk factors.
Managing and controlling underlying risk factors, such as hypertension, diabetes, and lifestyle choices, is crucial in preventing and minimizing the impact of microvascular ischemic disease. Regular medical check-ups and timely intervention are essential components of overall vascular health. Individuals experiencing symptoms or concerned about their risk should consult with a healthcare professional for proper assessment and guidance.
What are the risk factors for microvascular ischemic disease?
Several risk factors contribute to the development of microvascular ischemic disease, also known as small vessel disease (SVD). These risk factors can increase the likelihood of damage to the small blood vessels in various organs, with the brain being a common target. Identifying and addressing these risk factors is crucial for preventing and managing microvascular ischemic disease. Here are some key risk factors:
- Hypertension (High Blood Pressure):
- Chronic high blood pressure is a major risk factor for microvascular ischemic disease. Elevated blood pressure can lead to structural changes in the small blood vessels, making them more susceptible to damage.
- Aging:
- The risk of microvascular ischemic disease increases with age. Aging is associated with changes in blood vessels, including reduced elasticity and increased vulnerability to damage.
- Diabetes:
- Individuals with diabetes are at an increased risk of microvascular complications. Elevated blood sugar levels can lead to endothelial dysfunction and structural changes in small vessels.
- Smoking:
- Tobacco smoke contains harmful substances that can damage blood vessels. Smoking is a significant risk factor for small vessel disease and can contribute to the development of microvascular ischemic disease.
- Hyperlipidemia (High Cholesterol):
- Elevated levels of cholesterol and triglycerides in the blood can contribute to atherosclerosis, narrowing blood vessels and increasing the risk of microvascular complications.
- Cardiovascular Disease:
- Individuals with a history of cardiovascular diseases, such as coronary artery disease, may be at an increased risk of microvascular ischemic disease.
- Genetic Factors:
- There may be a genetic predisposition to small vessel disease. Individuals with a family history of vascular disorders may have an increased risk.
- Lifestyle Factors:
- Sedentary lifestyle, poor diet, and obesity are associated with an increased risk of vascular diseases, including microvascular ischemic disease.
- Gender:
- Some studies suggest that men may be at a slightly higher risk than women, particularly for coronary microvascular disease. However, the impact of gender can vary.
- Ethnicity:
- There may be variations in the prevalence of microvascular ischemic disease among different ethnic groups. However, individual risk varies, and the impact of ethnicity is complex.
- Chronic Kidney Disease:
- Individuals with chronic kidney disease may have an increased risk of microvascular complications.
It’s important to recognize that these risk factors often interact, and addressing multiple risk factors simultaneously is essential for effective prevention and management. Lifestyle modifications, such as maintaining a healthy diet, engaging in regular physical activity, quitting smoking, and managing chronic conditions like hypertension and diabetes, play a significant role in reducing the risk of microvascular ischemic disease. Regular medical check-ups and consultations with healthcare professionals can help assess individual risk and tailor preventive strategies accordingly.
What are the symptoms of microvascular ischemic disease?
The symptoms of microvascular ischemic disease, also known as small vessel disease (SVD), can vary depending on the organs affected. This condition is often associated with damage to the small blood vessels, particularly in the brain, and the symptoms may be related to impaired blood flow in these vessels. Common symptoms of microvascular ischemic disease include:
- Cognitive Impairment:
- Memory loss
- Difficulty concentrating
- Slowed thinking
- Executive function deficits
- Mood and Emotional Changes:
- Mood swings
- Depression
- Irritability
- Motor Function Issues:
- Problems with coordination and balance
- Gait disturbances
- Difficulty with fine motor skills
- Headaches:
- Chronic headaches, sometimes described as tension-type headaches
- Urinary Symptoms:
- Incontinence or urgency
- Visual Changes:
- Blurred vision
- Visual disturbances
- Fatigue:
- Generalized fatigue or a sense of tiredness
It’s important to note that the symptoms can be nonspecific and may overlap with other neurological or medical conditions. Additionally, not everyone with microvascular ischemic disease may experience noticeable symptoms, especially in the early stages.
The cognitive symptoms, such as memory loss and difficulty concentrating, are often related to changes in blood flow affecting specific areas of the brain. Mood and emotional changes can result from the impact of vascular damage on brain function.
In some cases, microvascular ischemic disease may lead to small infarcts or lacunar strokes, which can cause focal neurological symptoms such as weakness, numbness, or difficulty speaking. However, the symptoms can vary widely among individuals.
If you or someone you know is experiencing symptoms suggestive of microvascular ischemic disease, it’s crucial to seek medical attention promptly. A healthcare professional can conduct a thorough evaluation, including medical history, physical examination, and imaging studies (such as magnetic resonance imaging or MRI) to assess the extent of vascular changes and determine an appropriate course of action.
Early detection and management of microvascular ischemic disease are essential for minimizing the impact on cognitive function and overall well-being. Treatment may involve addressing underlying risk factors, lifestyle modifications, and medications to manage symptoms and reduce the risk of further vascular complications.
Diagnosis and Tests
How is microvascular ischemic disease diagnosed?
Microvascular ischemic disease, also known as small vessel disease (SVD), is often diagnosed through a combination of clinical evaluation, medical history, and imaging studies. The diagnosis aims to assess the presence and extent of small blood vessel damage, particularly in the brain. Here are the key approaches used in the diagnosis of microvascular ischemic disease:
- Clinical Evaluation:
- A healthcare professional will conduct a thorough clinical assessment, including a detailed medical history and physical examination. They will inquire about symptoms such as cognitive changes, mood disturbances, motor function issues, and other relevant symptoms.
- Neurological Examination:
- A neurological examination may be performed to assess cognitive function, motor skills, coordination, and other neurological aspects that may be affected by microvascular ischemic disease.
- Imaging Studies:
- Magnetic Resonance Imaging (MRI): This imaging modality is commonly used to visualize the brain and detect structural changes, including white matter hyperintensities, small infarcts, and other signs of microvascular ischemic disease. Specialized sequences such as diffusion-weighted imaging (DWI) and fluid-attenuated inversion recovery (FLAIR) are often employed.
- Computed Tomography (CT) Scan: While less sensitive than MRI in detecting small vascular changes, a CT scan may be used to assess brain structure and identify certain abnormalities.
- Cerebral Angiography:
- In some cases, cerebral angiography may be performed to visualize the blood vessels in the brain. This may involve injecting a contrast dye into the blood vessels and using imaging techniques to observe blood flow.
- Cerebrospinal Fluid Analysis:
- In certain situations, a lumbar puncture (spinal tap) may be performed to analyze the cerebrospinal fluid. This is less common but may be done to rule out other potential causes of neurological symptoms.
- Blood Tests:
- Blood tests may be conducted to assess general health, screen for diabetes, evaluate cholesterol levels, and check for other factors that may contribute to vascular diseases.
- Neuropsychological Testing:
- Neuropsychological tests may be administered to evaluate cognitive function, memory, and other aspects of mental processing. These tests can provide additional information about the impact of microvascular ischemic disease on cognitive abilities.
It’s important to note that microvascular ischemic disease is often a diagnosis of exclusion, meaning that other potential causes of symptoms must be ruled out before arriving at the conclusion of small vessel disease. Additionally, the severity of imaging findings may not always correlate directly with the severity of symptoms.
The diagnostic process is individualized based on the patient’s specific symptoms, medical history, and the healthcare professional’s clinical judgment. Once diagnosed, management strategies can be implemented to address underlying risk factors, provide symptomatic relief, and promote overall vascular health. If you suspect microvascular ischemic disease or are experiencing symptoms, it’s essential to seek medical attention for a comprehensive evaluation and appropriate diagnostic testing
Management and Treatment
Can microvascular ischemic disease be reversed?
Microvascular ischemic disease, also known as small vessel disease (SVD), involves structural changes and damage to small blood vessels, particularly in the brain. As of my knowledge cutoff in January 2022, the changes associated with microvascular ischemic disease are generally considered irreversible. However, the progression of the disease and the impact on symptoms can often be managed with appropriate interventions. It’s important to note that the management strategies primarily focus on preventing further damage, addressing risk factors, and improving overall vascular health.
Management and Treatment Approaches:
- Addressing Underlying Risk Factors:
- Management of conditions such as hypertension, diabetes, and hyperlipidemia is crucial. Controlling these risk factors can help slow the progression of microvascular disease.
- Lifestyle Modifications:
- Adopting a healthy lifestyle, including a balanced diet, regular exercise, smoking cessation, and moderation of alcohol intake, can contribute to overall cardiovascular health.
- Medications:
- Depending on the specific symptoms and underlying conditions, healthcare professionals may prescribe medications. These may include antiplatelet agents (such as aspirin) to reduce the risk of blood clots, medications to control blood pressure, and other medications to manage associated symptoms.
- Cognitive Rehabilitation:
- Individuals experiencing cognitive impairment may benefit from cognitive rehabilitation programs, which involve exercises and strategies to enhance cognitive function and daily functioning.
- Physical Therapy:
- For individuals with motor function issues or gait disturbances, physical therapy can be beneficial. Physical therapists can work with individuals to improve coordination, balance, and strength.
- Regular Monitoring:
- Regular medical check-ups and monitoring are essential to assess the progression of the disease and make necessary adjustments to the treatment plan.
While the structural changes associated with microvascular ischemic disease may not be reversible, effective management can help improve quality of life, reduce the risk of complications, and slow the progression of the disease. The success of management strategies varies among individuals, and a personalized approach is often necessary.
It’s important for individuals diagnosed with microvascular ischemic disease to work closely with healthcare professionals to develop a comprehensive and individualized management plan. Early detection and intervention, along with consistent adherence to treatment recommendations, play crucial roles in optimizing outcomes.
Since medical knowledge evolves, and new research may become available, it’s advisable to consult with a healthcare professional for the most up-to-date information and guidance regarding microvascular ischemic disease management.
How is microvascular ischemic disease treated?
The treatment of microvascular ischemic disease, also known as small vessel disease (SVD), involves a multifaceted approach aimed at managing symptoms, preventing further damage, and addressing underlying risk factors. While the structural changes associated with microvascular ischemic disease are generally considered irreversible, effective management can significantly improve the quality of life and slow the progression of the disease. Treatment strategies may include:
- Management of Underlying Conditions:
- Hypertension Control: Strict blood pressure control is crucial in managing microvascular disease. Medications may be prescribed to lower and control blood pressure.
- Diabetes Management: For individuals with diabetes, maintaining optimal blood sugar levels is important. This may involve lifestyle modifications, medications, and insulin therapy.
- Hyperlipidemia Control: Managing cholesterol levels through lifestyle changes and medications may be recommended to reduce the risk of further vascular damage.
- Antiplatelet Therapy:
- Medications such as aspirin or other antiplatelet agents may be prescribed to reduce the risk of blood clots, which can contribute to vascular complications.
- Symptomatic Treatment:
- Depending on the symptoms experienced, medications may be prescribed to manage specific issues. For example, antidepressants or mood-stabilizing medications may be used for mood disturbances.
- Lifestyle Modifications:
- Healthy Diet: Adopting a heart-healthy diet that includes fruits, vegetables, whole grains, lean proteins, and low-fat dairy products can contribute to overall cardiovascular health.
- Regular Exercise: Engaging in regular physical activity, as recommended by healthcare professionals, can improve cardiovascular fitness and help manage associated symptoms.
- Smoking Cessation: Quitting smoking is essential to reduce further damage to blood vessels and improve overall health.
- Cognitive Rehabilitation:
- For individuals experiencing cognitive impairment, cognitive rehabilitation programs may be beneficial. These programs include exercises and strategies to improve memory, attention, and problem-solving skills.
- Physical Therapy:
- Physical therapy can be beneficial for individuals with motor function issues, gait disturbances, or balance problems. Physical therapists can provide exercises to improve coordination and strength.
- Regular Monitoring and Follow-Up:
- Regular medical check-ups and monitoring are important to assess the progression of the disease, manage medications, and make necessary adjustments to the treatment plan.
It’s crucial for individuals diagnosed with microvascular ischemic disease to work closely with healthcare professionals to develop and implement a comprehensive and individualized management plan. Treatment approaches may vary based on the specific symptoms, underlying conditions, and overall health of the individual.
It’s important to note that while treatment can effectively manage symptoms and slow the progression of the disease, complete reversal of the structural changes associated with microvascular ischemic disease is generally not achievable. Early detection, consistent medical follow-up, and adherence to treatment recommendations are key factors in optimizing outcomes.
Prevention
How can I reduce my risk?
How do I know if I’m at risk?
Reducing the risk of microvascular ischemic disease involves adopting a heart-healthy lifestyle, managing key risk factors, and being proactive about overall vascular health. While some risk factors, such as age, are not modifiable, many others can be addressed through lifestyle changes and medical management. Here are steps you can take to reduce your risk and indicators that may suggest an increased risk:
Risk Reduction Strategies:
- Manage Blood Pressure:
- Keep your blood pressure within a healthy range. If you have hypertension, work with your healthcare provider to monitor and control your blood pressure through lifestyle changes and, if necessary, medications.
- Control Diabetes:
- If you have diabetes, maintain optimal blood sugar levels through diet, exercise, and medication as prescribed by your healthcare provider.
- Manage Cholesterol Levels:
- Keep your cholesterol levels in check by adopting a heart-healthy diet, exercising regularly, and taking medications if prescribed.
- Quit Smoking:
- If you smoke, quitting is one of the most effective ways to reduce your risk of microvascular disease and other cardiovascular conditions.
- Adopt a Healthy Diet:
- Follow a balanced diet that includes fruits, vegetables, whole grains, lean proteins, and low-fat dairy products. Limit intake of saturated and trans fats, cholesterol, and sodium.
- Engage in Regular Physical Activity:
- Exercise regularly to improve cardiovascular fitness. Aim for at least 150 minutes of moderate-intensity aerobic exercise or 75 minutes of vigorous-intensity aerobic exercise per week, combined with muscle-strengthening activities.
- Maintain a Healthy Weight:
- Achieve and maintain a healthy weight through a combination of a balanced diet and regular physical activity.
- Limit Alcohol Intake:
- If you consume alcohol, do so in moderation. For most adults, moderate drinking is defined as up to one drink per day for women and up to two drinks per day for men.
Indicators of Increased Risk:
- Age:
- Microvascular ischemic disease is more common in older adults. The risk increases with age.
- Medical History:
- A history of cardiovascular diseases, strokes, or other vascular conditions may increase the risk.
- Family History:
- A family history of vascular disorders or microvascular disease may indicate a genetic predisposition.
- Hypertension:
- High blood pressure is a significant risk factor. Regular blood pressure monitoring is important.
- Diabetes:
- Individuals with diabetes are at an increased risk. Regular blood sugar monitoring and diabetes management are crucial.
- Smoking:
- Tobacco use is a major risk factor for vascular diseases, including microvascular ischemic disease.
- Lack of Physical Activity:
- Sedentary behavior and lack of regular exercise can contribute to cardiovascular risk.
- Unhealthy Diet:
- A diet high in saturated and trans fats, cholesterol, and sodium can contribute to vascular issues.
- Obesity:
- Being overweight or obese is associated with an increased risk of vascular diseases.
If you have concerns about your risk for microvascular ischemic disease, or if you have one or more of the risk factors mentioned above, it’s important to consult with a healthcare professional. They can assess your individual risk, provide personalized recommendations, and guide you in developing a preventive strategy tailored to your specific health profile. Regular health check-ups and screenings are important for maintaining vascular health and preventing potential complications.
Outlook / Prognosis
What is the outlook for microvascular ischemic disease?
The outlook for microvascular ischemic disease, also known as small vessel disease (SVD), can vary widely among individuals. The progression and impact of the disease depend on factors such as the severity of vascular changes, the presence of underlying risk factors, and the effectiveness of management strategies. Here are key points regarding the outlook and prognosis for microvascular ischemic disease:
- Heterogeneity of Presentation:
- Microvascular ischemic disease can manifest in various ways, and the clinical presentation is heterogeneous. Some individuals may experience noticeable symptoms, such as cognitive impairment or motor function issues, while others may have imaging evidence of small vessel changes without apparent symptoms.
- Management Strategies Influence Prognosis:
- Effective management of underlying risk factors and lifestyle modifications can positively influence the prognosis. Timely intervention, adherence to prescribed medications, and a commitment to a healthy lifestyle contribute to improved outcomes.
- Severity of Vascular Changes:
- The extent and severity of structural changes in the small blood vessels, as observed on imaging studies (e.g., MRI), can impact the prognosis. More extensive damage may be associated with a greater risk of complications.
- Individual Response to Treatment:
- The response to treatment varies among individuals. Some individuals may experience stabilization of symptoms and a slower progression of the disease with appropriate management, while others may continue to face challenges.
- Impact on Daily Functioning:
- Microvascular ischemic disease can affect various aspects of daily functioning, including cognitive abilities, mood, and motor function. The degree of impact on an individual’s life can influence the overall prognosis.
- Quality of Life:
- Effective management and a proactive approach to vascular health can contribute to a better quality of life for individuals with microvascular ischemic disease. Symptomatic relief, cognitive rehabilitation, and support for daily activities may enhance overall well-being.
- Prevention of Complications:
- By addressing underlying risk factors and adopting preventive measures, the risk of complications such as strokes or further vascular events can be minimized.
It’s important to note that microvascular ischemic disease is often a chronic condition, and while the disease itself may not be curable, its impact can be managed and its progression slowed. Regular medical follow-ups, ongoing monitoring, and adjustments to the treatment plan as needed are crucial components of long-term management.
Individuals diagnosed with microvascular ischemic disease should work closely with healthcare professionals to develop a comprehensive management plan tailored to their specific needs. Early detection, proactive intervention, and a commitment to a healthy lifestyle contribute to optimizing outcomes and maintaining vascular health. If you or someone you know is facing symptoms suggestive of microvascular ischemic disease, seeking timely medical attention is essential for a proper diagnosis and the initiation of appropriate management strategies.
can porn cause Chronic microvascular ischemic disorder?
As of my knowledge cutoff date in January 2022, there is no established scientific evidence or medical consensus linking the consumption of pornography to the development of chronic microvascular ischemic disorder or small vessel disease. Chronic microvascular ischemic disorder primarily involves structural changes and damage to the small blood vessels in the body, particularly in the brain.
The risk factors associated with microvascular ischemic disease are typically related to cardiovascular health, including conditions such as hypertension (high blood pressure), diabetes, smoking, hyperlipidemia (high cholesterol), and other factors that contribute to vascular damage. Lifestyle choices, genetics, and age also play significant roles in the development of small vessel disease.
It’s important to approach health-related questions with a critical mindset and rely on evidence-based information. If you have concerns about your vascular health or specific symptoms, it is recommended to consult with a healthcare professional who can provide personalized guidance based on a thorough evaluation of your medical history, risk factors, and symptoms.
Medical knowledge evolves, and new research may become available over time. Therefore, it’s advisable to stay informed about the latest scientific literature and consult with healthcare professionals for the most up-to-date and accurate information regarding health conditions.
This post was such a great resource. Thanks for sharing it with us!